Abdominal Aortic Aneurysm – The Silent Threat We Can Detect in Time
With deep gratitude, we present this special article by Dr. Dimcho Mihalev, a promising young vascular surgeon at the Heart and Brain Institute in Burgas. Dr. Mihalev kindly accepted our invitation to share his expert perspective on one of the most silent yet potentially fatal vascular diseases—abdominal aortic aneurysm. In this post, you will find clear medical information as well as practical advice for early diagnosis and prevention.

What Is the Aorta?
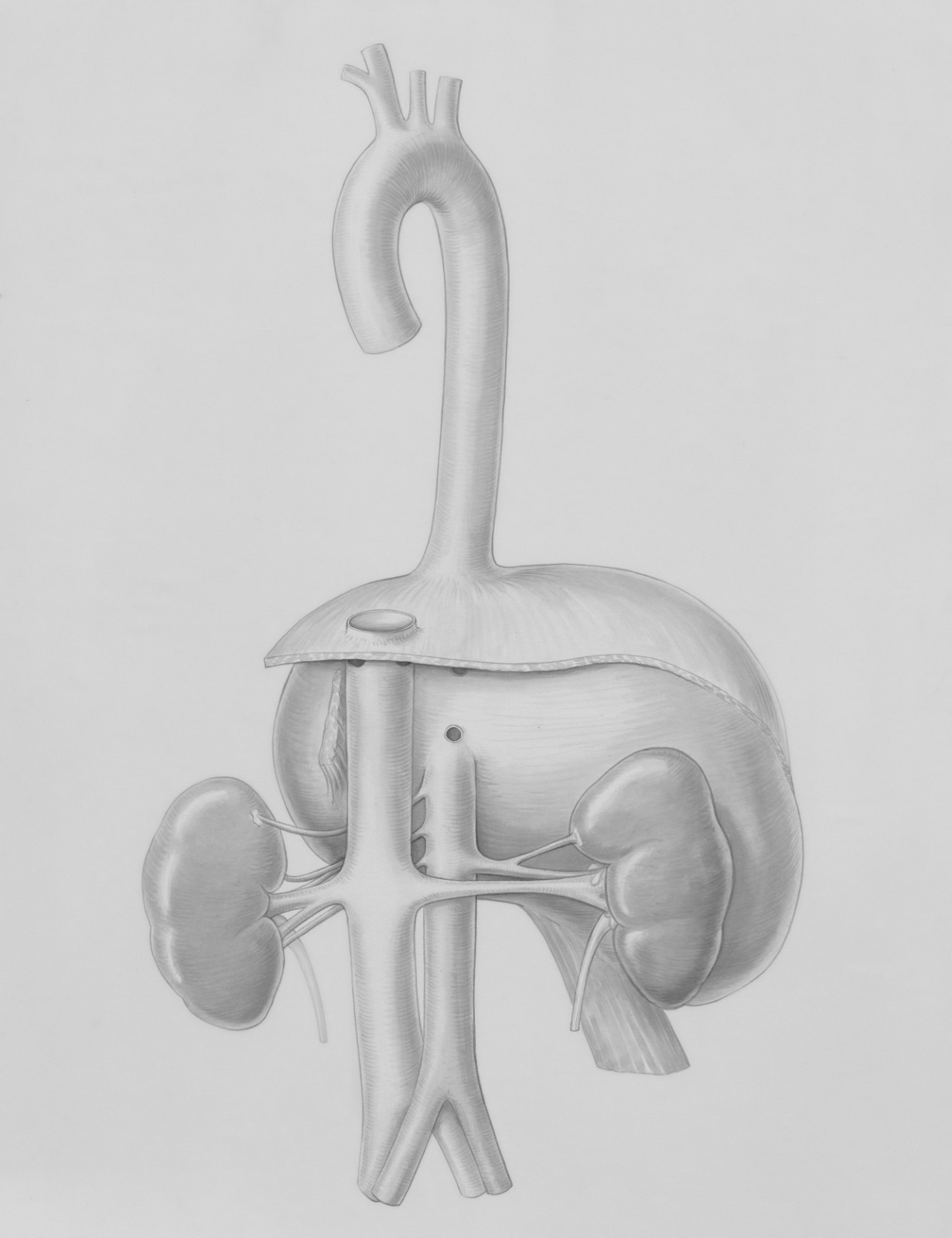
The aorta is the largest artery in the human body. It begins at the heart and ends by dividing into two iliac arteries, which supply blood to the legs. Anatomically, it’s divided into the ascending aorta, the descending aorta, and the abdominal aorta. An aneurysm is an abnormal enlargement of a blood vessel, most commonly affecting the arteries.
What Is an Abdominal Aortic Aneurysm?
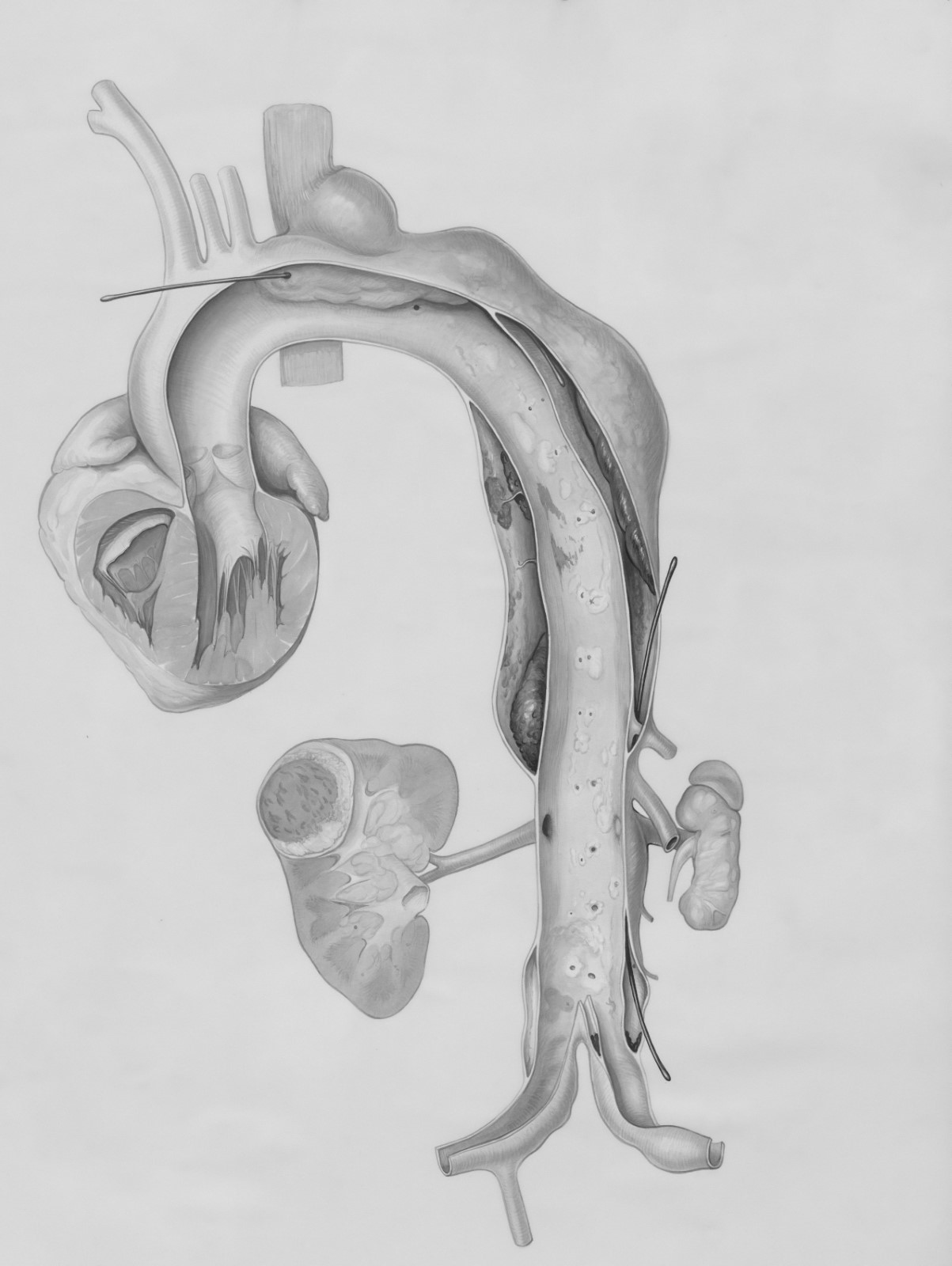
An abdominal aortic aneurysm (AAA) is a dilation of the abdominal portion of the aorta caused by weakening of its wall. Under the force of blood pressure, the weakened section bulges outward.
Why Is This Important?
As an aneurysm enlarges, the vessel wall becomes progressively weaker and may eventually rupture. A rupture causes massive internal bleeding into the abdominal cavity, leading to rapid onset of shock and potentially death if not treated immediately.
Risk Factors
Some individuals face higher risk, including those with:
-
Age over 65
-
Current or former smokers
-
Male sex
-
High blood pressure
-
Family history of aneurysm

Symptoms
Most AAAs are asymptomatic until rupture. Yet, large aneurysms can sometimes produce:
-
A pulsatile mass felt in the abdomen
-
Dull or throbbing abdominal pain radiating to the back
-
“Blue toe” syndrome (purple discoloration in toes)
Rupture causes sudden, severe abdominal pain, dizziness, weakness, and often loss of consciousness—an absolute emergency requiring immediate medical attention.

How Is It Detected?
AAAs are often discovered incidentally during an abdominal ultrasound exam—for example, during evaluations by a gastroenterologist, urologist, gynecologist, or radiologist. Confirmatory imaging (CT angiography) helps a vascular surgeon assess aneurysm size and decide on surveillance versus intervention.

Can We Prevent It?
You can reduce your risk by addressing modifiable factors:
-
Quit smoking
-
Control blood pressure
-
Maintain a healthy weight
-
Undergo regular vascular checkups, especially if over 65

How Is It Treated?
Treatment depends on aneurysm size:
-
Small aneurysms (<5.5 cm): Periodic monitoring and risk-factor management.
-
Large aneurysms (>5.5 cm): Repair is recommended to prevent rupture. Options include open surgical repair with a synthetic graft or endovascular repair with stent grafts. Both aim to divert blood flow through the graft or stent, relieving pressure on the weakened aortic wall.

Conclusion
The abdominal aortic aneurysm truly deserves the nickname “silent killer”—often symptomless until catastrophe strikes. The good news is that modern imaging and timely specialist consultation make it manageable. On behalf of the entire DrGoGo team, we thank Dr. Dimcho Mihalev for his valuable contribution and urge you to monitor your health, especially if you belong to a risk group. Early detection and prevention can save your life.

DrGoGo
Your companion on the path to informed, responsible health care.
Medical Disclaimers and Responsibilities
-
Educational Purpose Only
The information in this article is for general educational and informational purposes only. It does not replace consultation, diagnosis, or treatment by a qualified medical professional.
-
Not Medical Advice
If you experience symptoms or have concerns about an abdominal aortic aneurysm or any health condition, seek prompt evaluation by your primary care physician, cardiologist, vascular surgeon, or another qualified healthcare provider.
-
Individual Variability
Each person is unique; risk factors and appropriate prevention or treatment strategies may vary. Do not apply this advice without a personalized medical assessment.
-
Treatment Decisions
Decisions regarding surveillance, medications, or surgery must be made by a qualified vascular surgeon based on clinical and imaging findings.
-
Liability
Neither the DrGoGo team nor the article’s author, Dr. Dimcho Mihalev, is responsible for outcomes resulting from self-interpretation or application of this information.
-
Information Currency
Medical knowledge and guidelines evolve. This content is accurate as of publication; always verify the latest recommendations.
-
No Financial or Professional Affiliation
This article was published at the initiative of DrGoGo and reflects Dr. Mihalev’s voluntary expertise. Neither DrGoGo nor the author receives financial support, sponsorship, or direction from the Heart and Brain Institute—Burgas—or any other healthcare institution.


Comments